Congenital Talipes Equinovarus (Clubfoot)
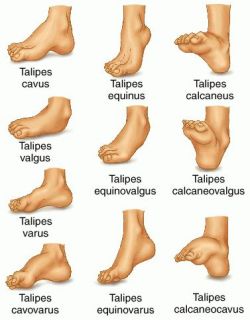
Congenital clubfoot is a deformity in which the entire foot is inverted, the heel is drawn up, and the forefoot is adducted.
What is Congenital Talipes Equinovarus?
Congenital talipes equinovarus or clubfoot is usually evident at birth.
- The Latin talus, meaning ankle, and pes, meaning foot, make up the word talipes, which is used in connection with many foot deformities.
- Clubfoot was depicted in Egyptian hieroglyphs and was described by Hippocrates around 400 bc; he advised treatment with manipulation and bandages, ‘manipulate the foot as if holding a wax model, not by force, but gently’.
- The Pirani, Goldner, Diméglio, Hospital for Joint Diseases (HJD), and Walker classifications have been published, but no classification system is universally used.
Pathophysiology
Various theories of the pathogenesis of clubfoot have been advanced.

- With respect to neurogenic factors, histochemical abnormalities have been found in posteromedial and peroneal muscle groups of patients with clubfeet.
- This is postulated to be due to innervation changes in intrauterine life secondary to a neurologic event, such as a stroke leading to mild hemiparesis or paraparesis.
- Retracting fibrosis (or myofibrosis) may occur secondary to increased fibrous tissue in muscles and ligaments.
- In fetal and cadaveric studies, Ponseti also found the collagen in all of the ligamentous and tendinous structures (except the Achilles [calcaneal] tendon), and it was very loosely crimped and could be stretched.
- The Achilles tendon, on the other hand, was made up of tightly crimped collagen and was resistant to stretching; Zimny et al found myoblasts in medial fascia on electron microscopy and postulated that they cause medial contracture.
Causes
The true etiology of congenital clubfoot is unknown.
- Extrinsic factors. Extrinsic associations include teratogenic agents (e.g., sodium aminopterin), oligohydramnios, and congenital constriction rings.
- Genetic factors. Genetic associations include Mendelian inheritance (eg, diastrophic dwarfism; autosomal recessive pattern of clubfoot inheritance).
- Cytogenic factors. Cytogenetic abnormalities (e.g., congenital talipes equinovarus [CTEV]) can be seen in syndromes involving chromosomal deletion; it has been proposed that idiopathic CTEV in otherwise healthy infants is the result of a multifactorial system of inheritance.
Statistics and Incidences
The incidence of clubfoot differ among ethnicities.

- The incidence of clubfoot is approximately 1 case per 1000 live births in the United States.
- The male-to-female ratio has been reported to be 2:1; bilateral involvement is found in 30-50% of cases; a 2017 study by Zionts et al found that severity did not differ significantly by either sex or bilaterality, though patients with bilateral clubfoot had a wider range of severity.
- There is a 10% chance of a subsequent child being affected if the parents already have a child with a clubfoot.

- Parker et al pooled data from several birth defects surveillance programs (6139 cases of clubfoot) to better estimate the prevalence of clubfoot and investigate its risk factors; the overall prevalence of clubfoot was 1.29 per 1000 live births, with figures of 1.38 among non-Hispanic whites, 1.30 among Hispanics, and 1.14 among non-Hispanic blacks or African Americans.
- Maternal age, parity, education, and marital status were significantly associated with clubfoot, along with maternal smoking and diabetes.
Clinical Manifestations
Most infants who have clubfoot have no identifiable genetic, syndromal, or extrinsic cause.
- Foot abnormality. The ankle is in equinus, and the foot is supinated (varus) and adducted (a normal infant foot usually can be dorsiflexed and everted, so that the foot touches the anterior tibia).
- Bone displacement. The navicular is displaced medially, as is the cuboid.
- Contractures. Contractures of the medial plantar soft tissues are present; not only is the calcaneus in a position of equinus, but also the anterior aspect is rotated medially and the posterior aspect laterally.
- Empty heel. The heel is small and empty; the heel feels soft to the touch (akin to the feel of the cheeks); as the treatment progresses, it fills in and develops a firmer feel (akin to the feel of the nose or of the chin).
Assessment and Diagnostic Findings

Occasionally, radiographs are necessary to diagnose clubfeet associated with tibial hemimelia.
- Radiographs. Talocalcaneal parallelism is the radiographic feature of clubfeet; the anteroposterior (AP) view is taken with the foot in 30° of plantarflexion and the tube at 30° from vertical. The lateral view is taken with the foot in 30° of plantarflexion.
Medical Management
The aims of medical therapy for clubfoot are to correct the deformity early and fully and to maintain the correction until growth stops.
- The Pirani scoring system. The Pirani scoring system, devised by Shafiq Pirani, MD, of Vancouver, BC, consists of six categories, three in the hindfoot and three in the midfoot; the Pirani scoring system can be used to identify the severity of the clubfoot and to monitor the correction.
- Traditional nonoperative treatment. With traditional nonoperative treatment, splintage begins at 2-3 days after birth; merely bring the foot to the best position obtainable, and maintain this position either by strapping every few days or by changing casting weekly until either full correction is obtained or correction is halted by some irresistible force.
- The Ponseti method. This method was developed by Ignacio Ponseti, MD, of the University of Iowa; the premise of the method is based on Ponseti’s cadaveric and clinical observations; a 2014 Cochrane review found this approach to yield significantly better results than either the Kite method or a traditional approach, though it noted that the quality of the evidence was not high; a study by Dragoni et al suggested that this approach may be effective for treatment of rigid residual deformity of congenital clubfoot after walking age.
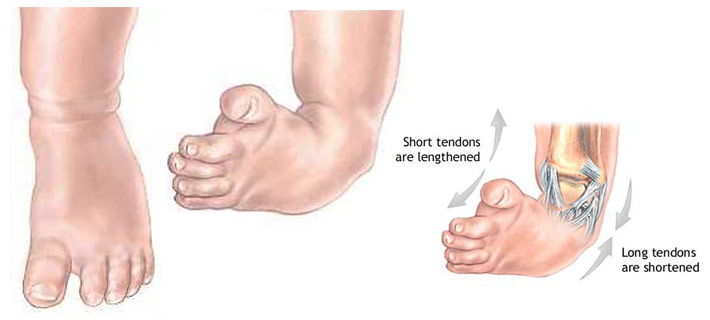
Surgical Management
Although it is sometimes recommended that idiopathic clubfoot is treated as soon as possible, this condition does not constitute an orthopedic emergency.

- Surgical clubfoot release. In the past, clubfoot surgery was performed in a way that did not differentiate severity; the same procedure was performed for all patients; Bensahel proposed a more individualized approach (ie, addressing only the structures that are required are released); the surgery is tailored to the deformity.
Nursing Management
Nursing care of an infant with clubfoot include the following:
Nursing Assessment
Assessment of a child with clubfoot include:
- History. Seek a detailed family history of clubfoot or neuromuscular disorders, and perform a general examination to identify any other abnormalities.
- Physical exam. Examine the feet with the child prone, with the plantar aspect of the feet visualized, and supine to evaluate internal rotation and varus; if the child can stand, determine whether the foot is plantigrade, whether the heel is bearing weight, and whether it is in varus, valgus, or neutral.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Disturbed body image related to permanent alteration in structure and/or function.
- Deficient knowledge related to the condition, prognosis, treatment, self-care, and discharge needs.
- Risk for peripheral neurovascular dysfunction related to mechanical compression (cast or brace).
- Risk for impaired skin integrity related to cast application, traction or surgery.
- Risk for impaired parenting related to maladaptive coping strategies secondary to diagnosis of talipes deformity.
Nursing Care Planning and Goals
The major nursing care planning goals for patients with congenital talipes equinovarus (clubfoot) are:
- Parents verbalize acceptance of self in the situation
- Family/SO discuss about situation and changes that would have occurred.
- Parents develop realistic goals/plans for the future.
- Parents explain disease state, recognizes the need for medications and understands treatments.
- Parents demonstrate how to incorporate new health regimen into lifestyle.
- Parents exhibit ability to deal with health situation and remain in control of life.
- Parents demonstrate an understanding of plan to heal tissue and prevent injury.
- Parents describe measures to protect and heal the tissue, including wound care.
Nursing Interventions
Nursing interventions for the child are:
- Protect skin integrity. Monitor site of impaired tissue integrity at least once daily for color changes, redness, swelling, warmth, pain, or other signs of infection; monitor patient’s skin care practices, noting type of soap or other cleansing agents used, temperature of water, and frequency of skin cleansing; and provide gloves or clip the nails if necessary to avoid damaging the skin with scratches.
- Promote acceptance of body image. Acknowledge and accept an expression of feelings of frustration, dependency, anger, grief, and hostility; support verbalization of positive or negative feelings about the actual or perceived loss; and be realistic and positive during treatments, in health teaching, and in setting goals within limitations.
- Provide health education. Include the parents in creating the teaching plan, beginning with establishing objectives and goals for learning at the beginning of the session; provide clear, thorough, and understandable explanations and demonstrations; and render positive, constructive reinforcement of learning.
Evaluation
Goals are met as evidenced by:
- Parents verbalized acceptance of self in situation
- Family/SO discussed about situation and changes that would have occurred.
- Parents developed realistic goals/plans for the future.
- Parents explained disease state, recognizes need for medications, and understands treatments.
- Parents demonstrated how to incorporate new health regimen into lifestyle.
- Parents exhibited ability to deal with health situation and remain in control of life.
- Parents demonstrated an understanding of plan to heal tissue and prevent injury.
- Parents described measures to protect and heal the tissue, including wound care.
Documentation Guidelines
Documentation in a child with clubfoot include:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Characteristics of the skin.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Practice Quiz: Congenital Talipes Equinovarus (Clubfoot)
Here’s a 5-item quiz for Congenital Talipes Equinovarus (Clubfoot) study guide. Please visit our nursing test bank page for more NCLEX practice questions.
1. Parents brought their 2-week-old infant to a clinic for treatment after a diagnosis of clubfoot made at birth. Which statement by the parents indicates a need for further teaching regarding this disorder?
A. “I realize my infant will require follow-up care until fully grown.”
B. “Treatment needs to be started as soon as possible.”
C. “I need to come to the clinic every week with my infant for the casting.”
D. “I need to bring my infant back to the clinic in 1 month for a new cast.”
1. Answer: D. “I need to bring my infant back to the clinic in 1 month for a new cast.”
- Option D: Clubfoot is a complex deformity of the ankle and foot that includes forefoot adduction, midfoot supination, hindfoot varus, and ankle equinus; the defect may be unilateral or bilateral.
- Option A: Because clubfoot can recur, all children with clubfoot require long-term interval follow-up until they reach skeletal maturity to ensure an optimal outcome.
- Option B: Treatment for clubfoot is started as soon as possible after birth.
- Option C: Serial manipulation and casting are performed at least weekly.
2. The nurse prepares a list of home care instructions for the parents of a child who has a plaster cast applied to the left forearm. Which instructions should be included on the list? Select all that apply.
A. Use the fingertips to lift the cast while it is drying.
B. Keep small toys and sharp objects away from the cast.
C. Use a padded ruler or another padded object to scratch the skin under the cast if it itches.
D. Place a heating pad on the lower end of the cast and over the fingers if the fingers feel cold.
E. Elevate the extremity on pillows for the first 24 to 48 hours after casting to prevent swelling.
F. Contact the healthcare provider (HCP) if the child complains of numbness or tingling in the extremity.
2. Answer: B, E, F.
- Options B & C: Small toys and sharp objects are kept away from the cast, and no objects (including padded objects) are placed inside the cast because of the risk of altered skin integrity.
- Option E: The extremity is elevated to prevent swelling, and the HCP is notified immediately if any signs of neurovascular impairment develop.
- Option F: Cold fingers could indicate neurovascular impairment, and the HCP should be notified.
- Option A: While the cast is drying, the palms of the hands are used to lift the cast. If the fingertips are used, indentations in the cast could occur and cause constant pressure on the underlying skin.
- Option D: A heating pad is not applied to the cast or fingers.
3. Nurse Christopher is caring for an infant with congenital clubfoot. After the final cast has been removed, which member of the healthcare team will most likely help the infant with leg and ankle exercises and provide his parents with a home exercise regimen?
A. Occupational therapist.
B. Recreational therapist.
C. Physical therapist.
D. Speech therapist.
3. Answer: C. Physical therapist.
- Option C: After the final cast has been removed, foot and ankle exercises may be necessary to improve range of motion.
- Options A, B, D: These therapists are not necessary for a child with clubfoot.
4. A client with clubfoot has a plaster-of-Paris cast applied to immobilize the fracture. Which action by the nurse indicates an understanding of a plaster-of-Paris cast? The nurse:
A. Allows 24 hours before bearing weight.
B. Dries the cast with a hairdryer.
C. Petals the cast.
D. Handles the cast with the fingertips.
4. Answer: A. Allows 24 hours before bearing weight.
- Option A: A plaster-of-Paris cast takes 24 hours to dry, and the client should not bear weight for 24 hours.
- Option B: The client should be told not to dry the cast with a hair dryer because this causes hot spots and could burn the client. This also causes unequal drying.
- Option C: Petaling a cast is covering the end of the cast with cast batting or a sock, to prevent skin irritation and flaking of the skin under the cast.
- Option D: The cast should be handled with the palms, not the fingertips.
5. A nurse provides discharge teaching to the parents of a newborn who has a cast in place for talipes equinovarus. Which of the following statements indicate a need for additional teaching? “We will…
A. Check the toes frequently for color and temperature changes.”
B. Bring the baby to the doctor next week for a cast change.”
C. Perform a range of motion exercises to the affected foot.”
D. Avoid tub baths while the cast is in place.”
5. Answer: C. Perform a range of motion exercises to the affected foot.”
- Option C: Range of motion exercises are not performed while the cast is in place. The purpose of the cast is to gradually stretch the skin and structures on the medial side of the foot to correct the clubfoot.
- Option A: Circulation of the toes is assessed frequently throughout the day including color and temperature of the toes. Pale, cyanotic and cold toes should be reported immediately.
- Option B: The cast is removed every few days for 1 to 2 weeks and then at 1 to 2-week intervals. This is continued until maximum correction is achieved, typically within 8 to 12 weeks.
- Option D: Tub baths are avoided while the cast is in place. The cast should be kept clean and dry. This statement does not require additional teaching.
See Also
Related topics to this study guide:
- Pediatric Nursing Study Guides
- Nursing Notes: Study Guides for Various Topics
- Pediatric Nursing NCLEX Practice Questions
Further Reading
Recommended resources and books for pediatric nursing:

