Down Syndrome (Trisomy 21)
Down syndrome is the most common chromosomal anomaly, occurring in about 1 in 700 to 800 births.
What is Down Syndrome?
- It is primarily caused by trisomy of chromosome 21, which gives rise to multiple systemic complications as part of the syndrome.
- Langdon Down first described the condition in 1866, but its cause was a mystery for many years.
- In 1932, it was suggested that a chromosomal anomaly might be the cause, but the anomaly was not demonstrated until 1959.
Pathophysiology
Two different hypotheses have been proposed to explain the mechanism of gene action in Down syndrome: developmental instability (ie, loss of chromosomal balance) and the so-called gene-dosage effect.
- According to the gene-dosage effect hypothesis, the genes located on chromosome 21 have been overexpressed in cells and tissues of Down syndrome patients, and this contributes to the phenotypic abnormalities.
- Molecular analysis reveals that the 21q22.1-q22.3 region, also known as the Down syndrome critical region (DSCR), appears to contain the gene or genes responsible for the congenital heart disease observed in Down syndrome.
- Abnormal physiologic functioning affects thyroid metabolism and intestinal malabsorption; patients with trisomy 21 have an increased risk of obesity; frequent infections are presumably due to impaired immune responses, and the incidence of autoimmunity, including hypothyroidism and rare Hashimoto thyroiditis, is increased.
- Patients with Down syndrome have decreased buffering of physiologic reactions, resulting in hypersensitivity to pilocarpine and abnormal responses on sensory-evoked electroencephalographic (EEG) tracings.
- Decreased buffering of metabolic processes results in a predisposition to hyperuricemia and increased insulin resistance.
- Children with Down syndrome are predisposed to developing leukemia, particularly transient myeloproliferative disorder and acute megakaryocytic leukemia.
- Musculoskeletal manifestations in patients with Down syndrome include reduced height, atlantooccipital and atlantoaxial hypermobility, and vertebral malformations of the cervical spine.
- About 5% of patients with Down syndrome have GI manifestations, including duodenal atresia, Hirschsprung disease, and celiac disease.
Statistics and Incidences
Down syndrome have been observed in nearly all countries and races.

- Each year, approximately 6000 children are born with Down syndrome.
- Down syndrome accounts for about one-third of all moderate and severe mental handicaps in school-aged children.
- The prevalence of Down syndrome worldwide has increased because of increases in lifespan in the last few decades.
- The characteristic morphologic features will be obvious in children older than 1 year.
- On rare occasions, the disease can be observed in a few members of a family; the risk for recurrence of Down syndrome in a patient’s siblings also depends on maternal age.
- The male-to-female ratio is slightly higher (approximately 1.15:1) in newborns with Down syndrome, but this effect is restricted to neonates with free trisomy 21.
- Perhaps 50% of female patients with trisomy 21 are fertile, and these females have up to a 50% chance of having a live child who also has trisomy 21.
Causes
The cause of DS is not known, although several theories dominate.

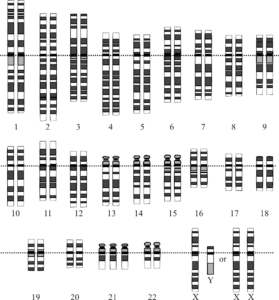
- Down syndrome is caused by the following 3 cytogenetic variants: three full copies of chromosome 21, a chromosomal translocation that results in 3 copies of the critical region for Down syndrome, and mosaicism.
- Full copies of trisomy 21. A free trisomy 21 results from nondisjunction during meiosis in one of the parents; this occurrence is correlated with advanced maternal and paternal age.
- Translocation. Translocation occurs when genetic material from chromosome 21 becomes attached to another chromosome, resulting in 46 chromosomes, with 1 chromosome having extra material from chromosome 21 attached.
- Mosaicism. Mosaicism is considered a postzygotic event (ie, one that occurs after fertilization); most cases result from a trisomic zygote with mitotic loss of one chromosome; as a result, two cell lines are found: one with a free trisomy and the other with a normal karyotype; this finding leads to great phenotypic variability, ranging from near normal to the classic trisomy 21 phenotype.
Clinical Manifestations
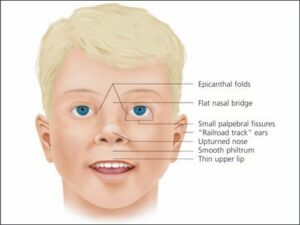
On physical examination, patients with trisomy 21 have characteristic craniofacial findings, such as the following:

- Flat occiput and a flattened facial appearance. This is mostly recognized by the time the child turns 1 year old or more.
- Small brachycephalic head. Brachycephaly or shortness of head is a common manifestation.
- Epicanthal folds. Epicanthal folds at the inner angle of the eyes are present.
- Flat nasal bridge. Another common manifestation is the short, flattened bridge of the nose of the child.
- Upward-slanting palpebral fissures. There is an “almond-shaped” appearance of the eyes.
- Brushfield spots. Brushfield spot is the speckling of the iris.
- Small nose and small mouth. The child is often identified as having a small nose and mouth.
- Protruding tongue. The protruding tongue is thick and fissured.
- Small and dysplastic ears. The child’s ears are also small and dysplastic.
- Generous nuchal skin. The child’s skin is dry, cracked, and fissured, and may be mottled.
Assessment and Diagnostic Findings
The diagnosis of Down syndrome is most commonly made by prenatal screening followed by definitive diagnostic testing.


- Laboratory studies. A complete blood count (CBC) with differential and bone marrow examination to rule out leukemia is indicated; thyroid-stimulating hormone (TSH) and thyroxine (T4) levels should be obtained at birth, at 6 and 12 months, and annually thereafter, to rule out hypothyroidism; and perform Papanicolaou smears every 1-3 years in sexually active women starting at the age of first intercourse.
- Cytogenetic studies. The clinical diagnosis of trisomy 21 should be confirmed with cytogenetic studies; karyotyping is essential to determine the risk of recurrence; in translocation Down syndrome, karyotyping of the parents and other relatives is required for proper genetic counseling.
- Fluorescence in situ hybridization (FISH). Fluorescence in situ hybridization (FISH) may be used for rapid diagnosis of trisomy 21; it can be successful in both prenatal diagnosis and diagnosis in the neonatal period; a FISH study will detect the presence of trisomy 21; however, it does not provide information about whether trisomy 21 is secondary to a translocation. therefore, a FISH test must be confirmed by a complete karyotype analysis.
- Prenatal screening and diagnosis. Prenatal screening using a combination of maternal serum biomarkers and ultrasonography can detect up to 95% of pregnancies affected by Down syndrome.
- Nuchal translucency (NT) scan. The nuchal translucency (NT) scan assesses the amount of fluid in the dorsum of the fetal neck and is best assessed at 11-14 weeks; an increased NT measurement is associated with an increased risk of genetic syndromes and can detect up to 70% of Down syndrome pregnancies.
- Amniocentesis. Amniocentesis, routinely performed at 14-16 weeks’ gestation, remains the criterion standard of invasive diagnostic tests. Testing for chromosomal disorders is 99.5% accurate.
- Chorionic villus sampling (CVS). Chorionic villus sampling (CVS) is performed at 10-13 weeks’ gestation; earlier testing is thought to be associated with a 1 in 300-1000 risk of fetal transverse limb deficiency, a small risk of maternal cell contamination, and a 0.5-1% risk of a fetal loss after the procedure.
Medical Management
Despite continued work, no notable medical treatments for intellectual disability associated with Down syndrome have been forthcoming. However, the dramatic improvements in medical care described below have greatly improved the quality of life for patients and increased their life expectancy.

- Surgical care. Timely surgical treatment of cardiac anomalies, detected during the newborn period or early infancy, may be necessary to prevent serious complications and is crucial for optimal survival; surgical intervention may be necessary to reduce atlantoaxial subluxation and to stabilize the upper segment of the cervical spine if neurologic deficits are clinically significant; congenital cataracts occur in about 3% of children and must be extracted soon after birth to allow light to reach the retina.
- Diet. No special diet is required unless celiac disease is present. A balanced diet and regular exercise are needed to maintain appropriate weight; feeding problems and failure to thrive usually improve after cardiac surgery.
- Activity. No restriction of activities is necessary; parents should be counseled about sports with an increased risk of spinal injuries, such as football, soccer, and gymnastics; advise the patient to exercise to maintain an appropriate weight.
Pharmacologic Management
The standard immunizations and well-child care should be provided. In addition, specific manifestations of the syndrome and associated conditions must be addressed, as follows:
- Digitalis and diuretics. Give digitalis and diuretics as necessary for cardiac management.
- Vaccines. Consider pneumococcal and influenza vaccination for children with chronic cardiac and respiratory disease; consider prophylactic palivizumab, since infants with Down syndrome are at high risk for hospitalization with a respiratory syncytial virus.
- Anticonvulsants. Administer anticonvulsants for tonic-clonic seizures or for infantile spasms (treat with steroids).
Nursing Management
Nursing management for a child with Down syndrome are:
Nursing Assessment
Assessment of a child with Down syndrome include:
- Physical assessment. The nurse should perform a thorough, systemic, head-to-toe assessment of the newborn.
- History. Nurses should obtain a history of mother’s pregnancy, birth history, and genetic testing.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Delayed growth and development related to impaired ability to achieve developmental tasks.
- Self-care deficit: bathing and hygiene, dressing, feeding, toileting related to cognitive impairment.
- Impaired verbal communication related to impaired receptive or expressive skills.
- Risk for infection related to decreased muscle tone and poor drainage of mucus.
Nursing Care Planning and Goals
The major goals for a child with Down syndrome are:
- The child will be able to perform motor, social, and/or expressive skills typical of age group within the scope of present capabilities.
- The child will perform self-care and self-control activities appropriate for age.
- The child will be able to establish a method of communication in which needs can be expressed.
- The child will be able to achieve timely wound healing; be free of purulent drainage or erythema, and be afebrile.
Nursing Interventions
Nursing interventions are:
- Provide adequate nutrition. Assess the child’ ability to swallow, provide information on the proper way of giving food, and provide good nutrition counseling.
- Frequent consultations are a must. Encourage parents to have the child’s hearing and vision checked regularly.
- Assess understanding of Down syndrome. Educate the parents about Down syndrome and the care of a child with the disease.
- Provide emotional support and motivation. The family caregiver needs support during these trying times; they need strong support and guidance from the time the child is born.
Evaluation
Goals are met as evidenced by:
- The child was able to perform motor, social, and/or expressive skills typical of age group within the scope of present capabilities.
- The child performed self-care and self-control activities appropriate for age.
- The child was able to establish a method of communication in which needs can be expressed.
- The child was able to achieve timely wound healing; be free of purulent drainage or erythema, and be afebrile.
Documentation Guidelines
Documentation in a child with Down’s syndrome include:
- Availability and use of support systems and community resources.
- Plan of care.
- Teaching plan.
- Attainment or progress toward desired outcomes.
- Deviations from normal parenting expectations.
Practice Quiz: Down Syndrome
Here’s a 5-item quiz for Down Syndrome study guide. Please visit our nursing test bank page
for more NCLEX practice questions.
A. Transverse palmar crease
B. Small tongue
C. Large nose
D. Restricted joint movement
1. Answer: A. Transverse palmar crease.
- Option A: Down syndrome is characterized by the following a transverse palmar crease (simian crease), separated sagittal suture, oblique palpebral fissures, small nose, depressed nasal bridge, high arched palate, excess and lax skin, wide spacing and plantar crease between the second and big toes, hyperextensible and lax joints, large protruding tongue, and muscle weakness.
- Option B: The child with Down syndrome has a protruding tongue that is thick and fissured.
- Option C: A small nose is manifested by children with Down syndrome.
- Option D: There is no restricted joint movement, rather the child has joint hyperextensibility or hyper-flexibility.
2. When planning care for an 8-year-old boy with Down syndrome, the nurse should:
A. Plan interventions according to the developmental levels of a 5-year-old because the child will have developmental delays.
B. Plan interventions according to the developmental level of a 7-year-old child because that’s the child’s age.
C. Direct all teaching to the parents because the child can’t understand.
D. Assess the child’s current developmental level and plan care accordingly.
2. Answer D. Assess the child’s current developmental level and plan care accordingly.
- Option D: Because children with Down syndrome can vary from mildly to severely mentally challenged, each child should be individually assessed.
- Options A & B: Nursing care plan should be planned according to the developmental age of a child with Down syndrome, not the chronological age.
- Option C: A child with Down syndrome is capable of learning, especially a child with mild limitations.
3. A nurse is monitoring the intake and output of a toddler with Down syndrome receiving furosemide (Lasix) IV. Which of the following method is the most appropriate for measuring the urine output?
A. Weighing the diaper.
B. Insert Foley catheter.
C. Ask the mother regarding the number of diaper changes.
D. Compare intake with output.
3. Answer: A. Weighing the diaper.
- Option A: The most appropriate method for measuring urine output of an infant is by weighing the diaper.
- Option B: Inserting a Foley catheter will provide the most accurate measurement but it gives the infant the risk of urinary tract infection.
- Options C & D: These will not provide the accurate measurement of the urine output.
4. Dustin who was diagnosed with Down syndrome has Hirschsprung‘s disease. He developed fever and watery explosive diarrhea. Which of the following would Nurse Joyce do first?
A. Monitor the child every 30 minutes.
B. Notify the physician immediately.
C. Administer an anti-diarrheal.
D. Nothing. (These findings are common in Hirschsprung’s disease.)
4. Answer: B. Notify the physician immediately.
- Option B: For the child with Hirschsprung’s disease, fever and explosive diarrhea indicate enterocolitis, a life-threatening situation. Therefore, the physician should be notified directly.
- Option A: The child is acutely ill and requires intervention, with monitoring more frequently than every 30 minutes.
- Option C: Generally, because of the intestinal obstruction and inadequate propulsive intestinal movement, antidiarrheals are not used to treat Hirschsprung’s disease.
- Option D: Hirschprung’s disease typically presents with chronic constipation.
5. A patient with Down syndrome recently started on phenytoin (Dilantin) to control simple complex seizures is seen in the outpatient clinic. Which information obtained during his chart review and assessment will be of greatest concern?
A. The gums appear enlarged and inflamed.
B. The white blood cell count is 2300/mm3.
C. Patient occasionally forgets to take the phenytoin until after lunch.
D. A patient wants to renew his driver’s license in the next month.
5. Answer: B. The white blood cell count is 2300/mm3.
- Option B: Leukopenia is a serious side effect of phenytoin and would require discontinuation of the medication.
- Options A, C, D: The other data indicate a need for further assessment and/or patient teaching, but will not require a change in medical treatment for the seizures.

