Peptic Ulcer Disease
Learn more about the nursing care management of patients with peptic ulcer disease in this study guide.
What is Peptic Ulcer Disease?
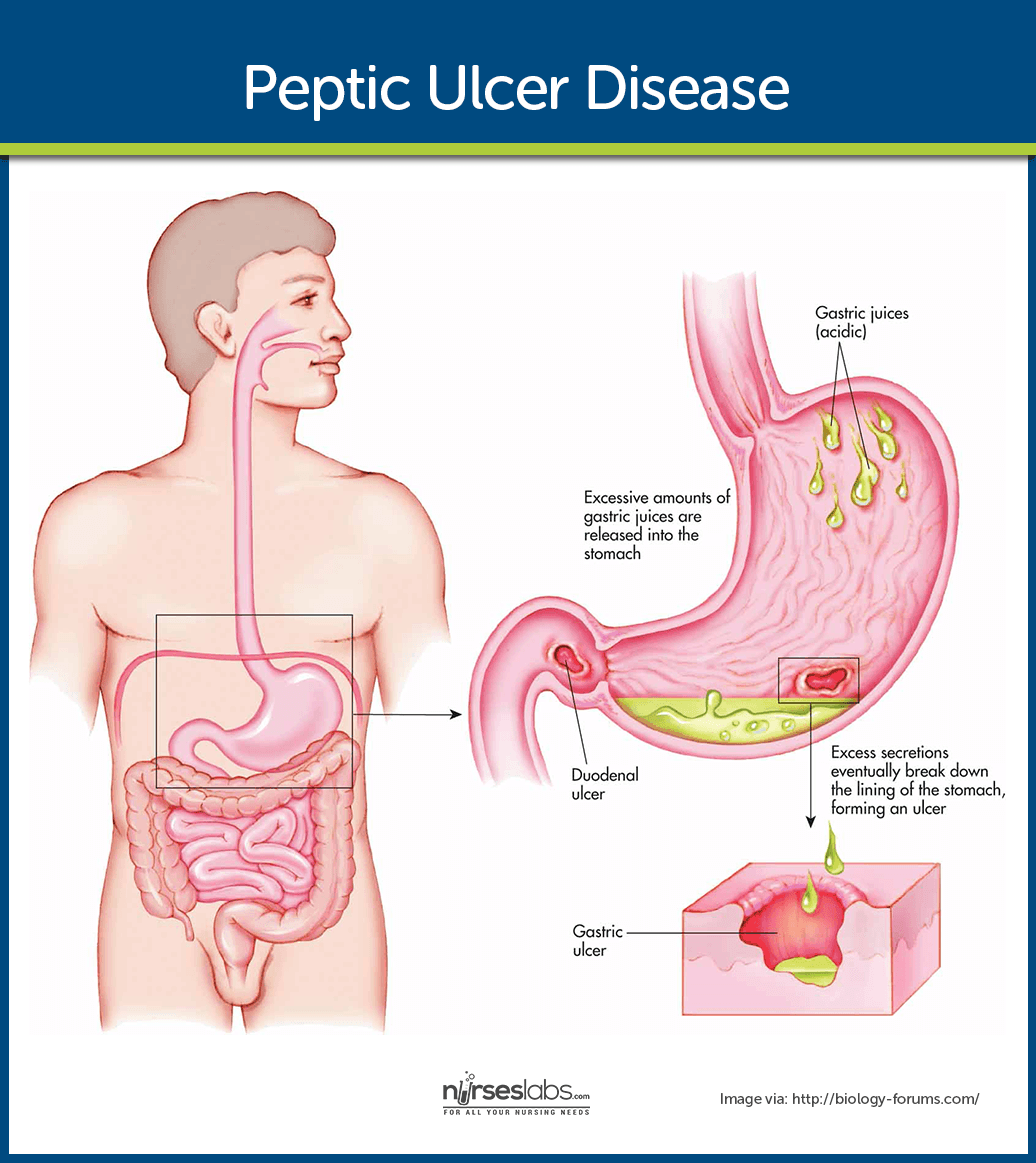
A peptic ulcer may be referred to as a gastric, duodenal, or esophageal ulcer, depending on its location.
- A peptic ulcer is an excavation that forms in the mucosal wall of the stomach, in the pylorus, in the duodenum, or in the esophagus.
- The erosion of a circumscribed area may extend as deep as the muscle layers or through the muscle to the peritoneum.
Classification
Peptic ulcer is classified into gastric, duodenal or esophageal ulcer.
- Duodenal ulcer. Peptic ulcers are more likely to occur in the duodenum than in the stomach.
- Esophageal ulcer. Esophageal ulcer occur as a result pf the backward flow of HCl from the stomach into the esophagus.
Pathophysiology
Peptic ulcers occur mainly in the gastroduodenal mucosa.
- Erosion. The erosion is caused by the increased concentration or activity of acid-pepsin or by decreased resistance of the mucosa.
- Damage. A damaged mucosa cannot secrete enough mucus to act as a barrier against HCl.
- Acid secretion. Patients with duodenal ulcers secrete more acid than normal, while patients with gastric ulcers tend to secrete normal or decreased levels of acid.
- Decreased resistance. Damage to the gastroduodenal mucosa results in decreased resistance to bacteria and thus infection from the H. pylori bacteria may occur.
Statistics and Epidemiology
Peptic ulcer disease may occur in both genders and in all ages.
- Peptic ulcer disease occurs with the greatest frequency in people between 40 and 60 years of age.
- It is relatively uncommon in women of childbearing age, but it has been observed in children and even in infants.
- After menopause, the incidence of peptic ulcers in women is almost equal to that in men.
Causes
There are three major causes of peptic ulcer disease: infection with H. pylori, chronic use of NSAIDs, and pathologic hypersecretory disorders (e.g., Zollinger-Ellison syndrome).
- Helicobacter pylori. Research has documented that peptic ulcers result from infection with the gram-negative bacteria H. pylori, which may be acquired through ingestion of food and water. H. pylori damage the mucous coating that protects the stomach and duodenum.
- Salicylates and NSAIDs. Encourages ulcer formation by inhibiting the secretion of prostaglandins.
- Various illnesses. Pancreatitis, hepatic disease, Crohn’s disease, gastritis, and Zollinger-Ellison syndrome are also known causes.
- Excess HCl. Excessive secretion of HCl in the stomach may contribute to the formation of peptic ulcers.
- Irritants. Ingestion of milk and caffeinated beverages and alcohol also increase HCl secretion. These contribute by accelerating gastric emptying time and promoting mucosal breakdown.
- Blood type. Gastric ulcers tend to strike people with type A blood while duodenal ulcers tend to afflict people with type O blood.
Clinical Manifestations
Symptoms of ulcer may last for a few days, weeks, months, and may disappear only to reappear, often without an identifiable cause.
- Pain. As a rule, the patient with an ulcer complains of dull, gnawing pain or a burning sensation in the midepigastrium or the back that is relieved by eating.
- Pyrosis. Pyrosis (heartburn) is a burning sensation in the stomach and esophagus that moves up to the mouth.
- Vomiting. Vomiting results from obstruction of the pyloric orifice, caused by either muscular spasm of the pylorus or mechanical obstruction from scarring.
- Constipation and diarrhea. Constipation or diarrhea may occur, probably as a result of diet and medications.
- Bleeding. 15% of patients may present with GI bleeding as evidenced by the passage of melena (tarry stools).
Complications
Possible complications may include:
- Hemorrhage. Hemorrhage, the most common complication, occurs in 10% to 20% of patients with peptic ulcers in the form of hematemesis or melena.
- Perforation and penetration. Perforation is the erosion of the ulcer through the gastric serosa into the peritoneal cavity without warning, while penetration is the erosion of the ulcer through the gastric serosa into adjacent structures.
- Pyloric obstruction. Pyloric obstruction occurs when the area distal to the pyloric sphincter becomes scarred and stenosed from spasm or edema or from scar tissue that forms when an ulcer alternately heals and breaks down.
Assessment and Diagnostic Findings
To establish the diagnosis of peptic ulcer, the following assessment and laboratory studies should be performed:
- Esophagogastroduodenoscopy. Confirms the presence of an ulcer and allows cytologic studies and biopsy to rule out H. pylori or cancer.
- Physical examination. A physical examination may reveal pain, epigastric tenderness, or abdominal distention.
- Barium study. A barium study of the upper GI tract may show an ulcer.
- Endoscopy. Endoscopy is the preferred diagnostic procedure because it allows direct visualization of inflammatory changes, ulcers, and lesions.
- Occult blood. Stools may be tested periodically until they are negative for occult blood.
- Carbon 13 (13C) urea breath test. Reflects activity of H. pylori.
Medical Management
Once the diagnosis is established, the patient is informed that the condition can be controlled.
- Pharmacologic therapy. Currently, the most commonly used therapy for peptic ulcers is a combination of antibiotics, proton pump inhibitors, and bismuth salts that suppress or eradicate the infection.
- Stress reduction and rest. Reducing environmental stress requires physical and psychological modifications on the patient’s part as well as the aid and cooperation of family members and significant others.
- Smoking cessation. Studies have shown that smoking decreases the secretion of bicarbonate from the pancreas into the duodenum, resulting in increased acidity of the duodenum.
- Dietary modification. Avoiding extremes of the temperature of food and beverages and overstimulation from consumption of meat extracts, alcohol, coffee, and other caffeinated beverages, and diets rich in cream and milk should be implemented.
Surgical Management
The introduction of antibiotics to eradicate H. pylori and of H2 receptor antagonists as a treatment for ulcers has greatly reduced the need for surgical interventions.
- Pyloroplasty. Pyloroplasty involves transecting nerves that stimulate the acid secretion and opening the pylorus.
- Antrectomy. Antrectomy is the removal of the pyloric portion of the stomach with anastomosis to either the duodenum or jejunum.
Nursing Management
The management of the patient with a peptic ulcer is as follows:.
Nursing Assessment
Nursing assessment includes:
Assessment for a description of pain.
- Assessment of relief measures to relieve the pain.
- Assessment of the characteristics of the vomitus.
- Assessment of the patient’s usual food intake and food habits.
Nursing Diagnosis
Based on the assessment data, the patient’s nursing diagnoses may include the following:
- Acute pain related to the effect of gastric acid secretion on damaged tissue.
- Anxiety related to an acute illness.
- Imbalanced nutrition related to changes in the diet.
- Deficient knowledge about prevention of symptoms and management of the condition.
Nursing Care Planning & Goals
Main Article: 5 Peptic Ulcer Disease Nursing Care Plans
The goals for the patient may include:
- Relief of pain.
- Reduced anxiety.
- Maintenance of nutritional requirements.
- Knowledge about the management and prevention of ulcer recurrence.
- Absence of complications.
Nursing Interventions
Nursing interventions for the patient may include:
Relieving Pain and Improving Nutrition
- Administer prescribed medications.
- Avoid aspirin, which is an anticoagulant, and foods and beverages that contain acid-enhancing caffeine (colas, tea, coffee, chocolate), along with decaffeinated coffee.
- Encourage patient to eat regularly spaced meals in a relaxed atmosphere; obtain regular weights and encourage dietary modifications.
- Encourage relaxation techniques.
Reducing Anxiety
- Assess what patient wants to know about the disease, and evaluate level of anxiety; encourage patient to express fears openly and without criticism.
- Explain diagnostic tests and administering medications on schedule.
- Interact in a relaxing manner, help in identifying stressors, and explain effective coping techniques and relaxation methods.
- Encourage family to participate in care, and give emotional support.
Monitoring and Managing Complications
If hemorrhage is a concern:
- Assess for faintness or dizziness and nausea, before or with bleeding; test stool for occult or gross blood; monitor vital signs frequently (tachycardia, hypotension, and tachypnea).
- Insert an indwelling urinary catheter and monitor intake and output; insert and maintain an IV line for infusing fluid and blood.
- Monitor laboratory values (hemoglobin and hematocrit).
- Insert and maintain a nasogastric tube and monitor drainage; provide lavage as ordered.
- Monitor oxygen saturation and administering oxygen therapy.
- Place the patient in the recumbent position with the legs elevated to prevent hypotension, or place the patient on the left side to prevent aspiration from vomiting.
- Treat hypovolemic shock as indicated.
If perforation and penetration are concerns:
- Note and report symptoms of penetration (back and epigastric pain not relieved by medications that were effective in the past).
- Note and report symptoms of perforation (sudden abdominal pain, referred pain to shoulders, vomiting and collapse, extremely tender and rigid abdomen, hypotension and tachycardia, or other signs of shock).
Home Management and Teaching Self-Care
- Assist the patient in understanding the condition and factors that help or aggravate it.
- Teach patient about prescribed medications, including name, dosage, frequency, and possible side effects. Also identify medications such as aspirin that patient should avoid.
- Instruct patient about particular foods that will upset the gastric mucosa, such as coffee, tea, colas, and alcohol, which have acid-producing potential.
- Encourage patient to eat regular meals in a relaxed setting and to avoid overeating.
- Explain that smoking may interfere with ulcer healing; refer patient to programs to assist with smoking cessation.
- Alert patient to signs and symptoms of complications to be reported. These complications include hemorrhage (cool skin, confusion, increased heart rate, labored breathing, and blood in the stool), penetration and perforation (severe abdominal pain, rigid and tender abdomen, vomiting, elevated temperature, and increased heart rate), and pyloric obstruction (nausea, vomiting, distended abdomen, and abdominal pain). To identify obstruction, insert and monitor nasogastric tube; more than 400 mL residual suggests obstruction.
Evaluation
Expected patient outcomes include:
- Relief of pain.
- Reduced anxiety.
- Maintained nutritional requirements.
- Knowledge about the management and prevention of ulcer recurrence.
- Absence of complications.
Discharge and Home Care Guidelines
The patient should be taught self-care before discharge.
- Factors that affect. The nurse instructs the patient about factors that relieve and those that aggravate the condition.
- Medications. The nurse reviews information about medications to be taken at home, including name, dosage, frequency, and possible side effects, stressing the importance of continuing to take medications even after signs and symptoms have decreased or subsided.
- Diet. The nurse instructs the patient to avoid certain medications and foods that exacerbate symptoms as well as substances that have acid-producing potential.
- Lifestyle. It is important to counsel the patient to eat meals at regular times and in a relaxed setting and to avoid overeating.
Documentation Guidelines
The focus of documentation should include:
- Client’s description of response to pain.
- Acceptable level of pain.
- Expectations of pain management.
- Prior medication use.
- Level of anxiety.
- Description of feelings (expressed and displayed).
- Awareness and ability to recognize and express feelings.
- Caloric intake.
- Individual cultural or religious restrictions and personal preferences.
- Learning style, identified needs, presence of learning blocks.
- Plan of care.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
- Long term needs.
Practice Quiz: Peptic Ulcer Disease
Here’s a 6-item quiz about the study guide. Please visit our nursing test bank for more NCLEX practice questions.
1. Peptic ulcers occur with the most frequency in those between the ages of:
A. 15 and 25 years.
B. 20 and 30 years.
C. 40 and 60 years.
D. 60 and 80 years.
2. The most common site for peptic ulcer formation is the:
A. Duodenum.
B. Esophagus.
C. Pylorus.
D. Stomach.
3. Peptic ulcer disease may be caused by which of the following?
A. Helicobacter pylori
B. Clostridium difficile
C. Candida albicans
D. Staphylococcus aureus
4. Pain control with peptic ulcer disease includes all of the following except:
A. promoting physical and emotional rest.
B. identifying stressful situations.
C. eating meals when desired.
D. administering medications that decrease gastric acidity.
5. A characteristic associated with peptic ulcer pain is a:
A. Burning sensation localized in the back or midepigastrium.
B. Feeling of emptiness that precedes meals from 1 to 3 hours.
C. Severe gnawing pain that increases in severity as the day progresses.
D. Combination of all of the above.
6. The most common complication of peptic ulcer disease that occurs in 10% to 20% of patients is:
A. Hemorrhage.
B. Intractable ulcer.
C. Perforation.
D. Pyloric obstruction.
Answers and Rationale
1. Answer: C. 40 and 60 years.
- C: Peptic ulcer disease occurs with the greatest frequency in people between 40 and 60 years of age.
- A, B, and D: These are incorrect.
2. Answer: A. Duodenum.
Peptic ulcers are more likely to occur in the duodenum.
3. Answer: A. Helicobacter pylori
Helicobacter pylori is considered to be the major cause of ulcer formation. Other choices are not related to ulcer formation.
4. Answer: C. eating meals when desired.
Meals should be regularly spaced in a relaxed environment. Choices A, B, and D are proper interventions in providing pain control.
5. Answer: A. Burning sensation localized in the back or midepigastrium.
- A: As a rule, the patient with an ulcer complains of dull, gnawing pain or a burning sensation in the midepigastrium or the back that is relieved by eating.
- B: A feeling of emptiness that precedes meals from 1 to 3 hours is not a characteristic associated with peptic ulcer pain.
- C: A severe gnawing pain that increases in severity as the day progresses is not a characteristic associated with peptic ulcer pain.
- D: Not all of the options are characteristics associated with peptic ulcer pain.
6. Answer: A. Hemorrhage.
- A: Hemorrhage, the most common complication, occurs in 10% to 20% of patients with peptic ulcers in the form of hematemesis or melena.
- B: Intractable ulcer is not the most common complication of peptic ulcer disease.
- C: Perforation is not the most common complication of peptic ulcer disease.
- D: Pyloric obstruction is not the most common complication of peptic ulcer disease.