Rheumatic Fever
Rheumatic fever is an inflammatory disease that can develop as a complication of inadequately treated strep throat or scarlet fever.
What is Rheumatic Fever?
Rheumatic fever is an inflammatory disease that can develop as a complication of inadequately treated strep throat or scarlet fever.
- Rheumatic fever (RF) is a systemic illness that may occur following group A beta-hemolytic streptococcal (GABHS) pharyngitis in children.
- Studies in the 1950s during an epidemic on a military base demonstrated 3% incidence of rheumatic fever in adults with streptococcal pharyngitis not treated with antibiotics.
- Strep throat and scarlet fever are caused by an infection with streptococcus bacteria.
Pathophysiology
Rheumatic fever develops in children and adolescents following pharyngitis with GABHS (ie, Streptococcus pyogenes).
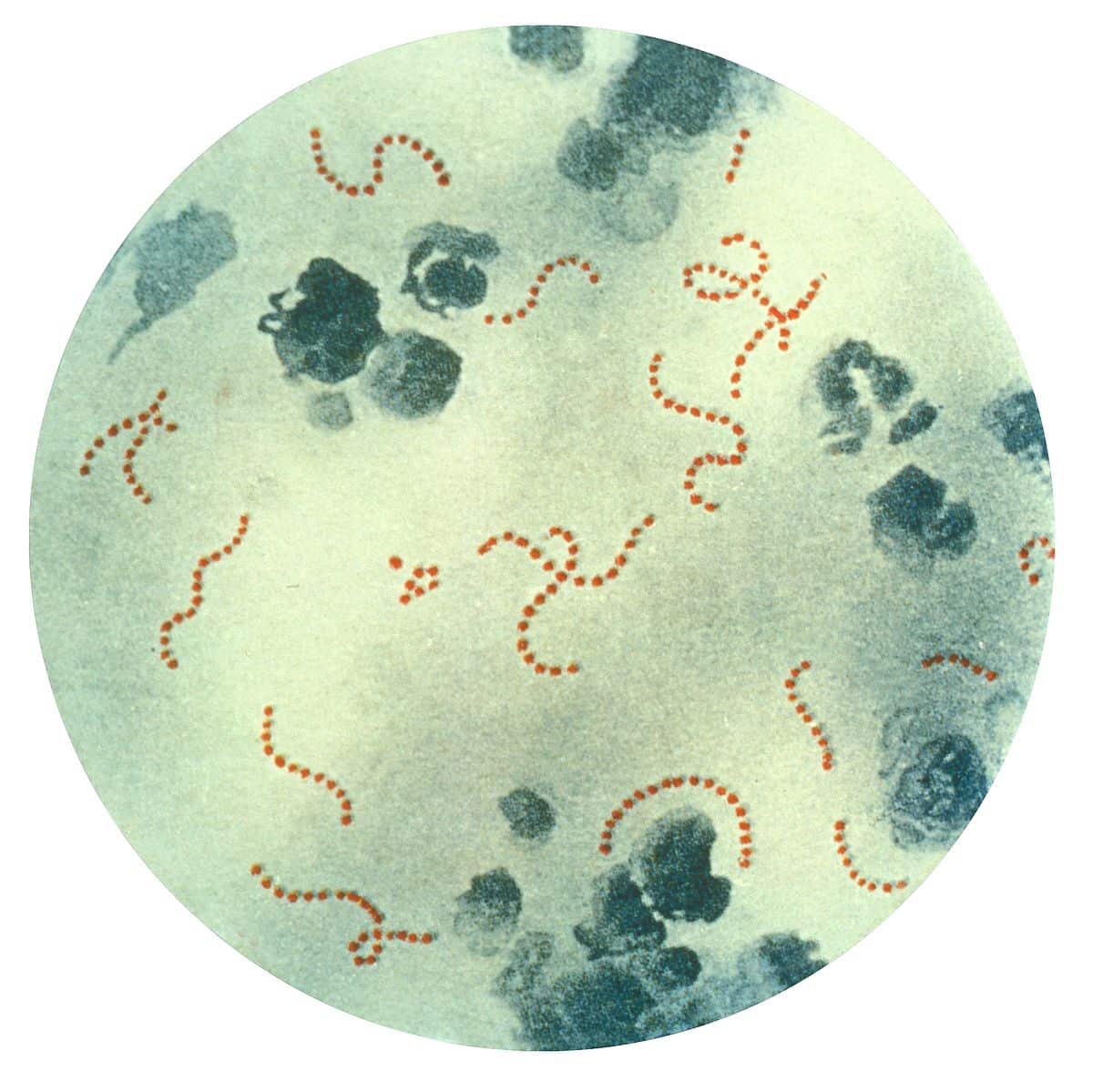
- The organisms attach to the epithelial cells of the upper respiratory tract and produce a battery of enzymes, which allows them to damage and invade human tissues.
- After an incubation period of 2-4 days, the invading organisms elicit an acute inflammatory response, with 3-5 days of sore throat, fever, malaise, headache, and elevated leukocyte count.
- In a small percentage of patients, infection leads to rheumatic fever several weeks after a sore throat has resolved; only infections of the pharynx have been shown to initiate or reactivate rheumatic fever.
- Direct contact with oral (PO) or respiratory secretions transmits the organism, and crowding enhances transmission; patients remain infected for weeks after symptomatic resolution of pharyngitis and may serve as a reservoir for infecting others.
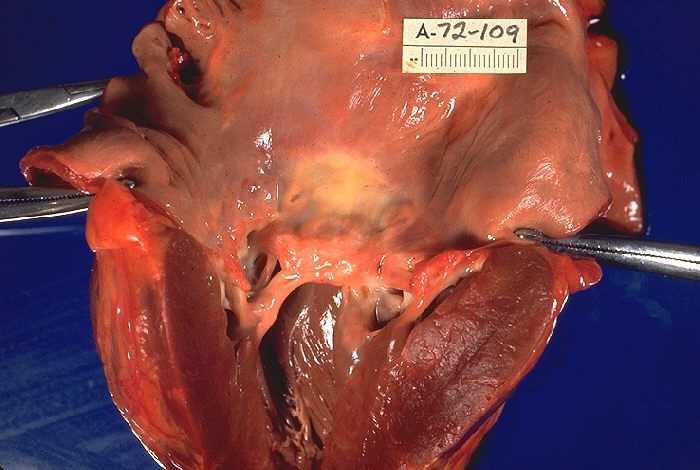
- Severe scarring of the valves develops during a period of months to years after an episode of acute rheumatic fever, and recurrent episodes may cause progressive damage to the valves.
- The mitral valve is affected most commonly and severely (65-70% of patients); the aortic valve is affected second most commonly (25%).
Statistics and Incidences
Rheumatic fever is most common in 5- to 15-year-old children, though it can develop in younger children and adults.

- The prevalence of RHD in the United States was less than 0.05 per 1000 population, with only rare regional outbreaks reported in Tennessee in the 1960s and in Utah, Ohio, and Pennsylvania in the 1980’s.
- However, a recent assessment of temporal trends of patients diagnosed with acute rheumatic fever in the United States from 2001-2011 showed that since 2001, national acute rheumatic fever admissions has steadily increased, with a peak in 2005, and decreased thereafter.
- Worldwide, there are over 15 million cases of RHD, with 282,000 new cases and 33,000 deaths from this disease each year.
- RHD is the major cause of morbidity from rheumatic fever and is the major cause of mitral insufficiency and stenosis in the United States and the world.
- Native Hawaiians and Maori (both of Polynesian descent) have a higher incidence of rheumatic fever; incidence of rheumatic fever in these patients is 13.4 per 100,000 hospitalized children per year, even with antibiotic prophylaxis of streptococcal pharyngitis.
- Rheumatic fever occurs in equal numbers in males and females; females with rheumatic fever fare worse than males and have a slightly higher incidence of chorea.
- Rheumatic fever is principally a disease of childhood, with a median age of 10 years; however, GABHS pharyngitis is uncommon in children younger than 3 years, and acute rheumatic fever is extremely rare in these younger children in industrialized countries.
Causes
Rheumatic fever is believed to result from an autoimmune response; however, the exact pathogenesis remains unclear.
- GABHS infection. Rheumatic fever only develops in children and adolescents following group A beta-hemolytic streptococcal (GABHS) pharyngitis, and only infections of the pharynx initiate or reactivate rheumatic fever.
- Molecular mimicry. So-called molecular mimicry between streptococcal and human proteins is felt to involve both the B and T cells of peripheral blood, with infiltration of the heart by T cells; some believe that an increased production of inflammatory cytokines is the final mechanism of the autoimmune reaction that causes damage to cardiac tissue in RHD.
- Streptococcal antigens. Streptococcal antigens, which are structurally similar to those in the heart, include hyaluronate in the bacterial capsule, cell wall polysaccharides (similar to glycoproteins in heart valves), and membrane antigens that share epitopes with the sarcolemma and smooth muscle.
- Decrease in regulatory T-cells. Decreased levels of regulatory T-cells have also been associated with rheumatic heart disease and with increased severity.

Clinical Manifestations
Revised in 1992 and again in 2016, the modified Jones criteria provide guidelines for making the diagnosis of rheumatic fever; the modified Jones criteria for recurrent rheumatic fever require the presence of 2 major, or 1 major and 2 minor, or 3 minor criteria for the diagnosis of rheumatic fever.
Major Diagnostic Criteria
- Carditis. Carditis in the child may be clinical and/or subclinical (echo).
- Polyarthritis. Monoarthritis or polyarthralgia are adequate to achieve major diagnostic criteria in Moderate/High-risk populations; for polyarthralgia exclusion of other more likely causes is also required.
- Chorea. Jerky, uncontrollable body movements (Sydenham chorea, or St. Vitus’ dance) — most often in the hands, feet, and face.
- Subcutaneous nodules. Small, painless bumps (nodules) beneath the skin.
- Erythema marginatum. Flat or slightly raised, painless rash with a ragged edge.
Minor Diagnostic Criteria
- Fever. Fever of ≥38.5°C ( ≥38°C to achieve a minor diagnostic criteria in Moderate/High-risk populations.
- Polyarthralgia. Painful and tender joints — most often in the knees, ankles, elbows, and wrists.
- Prolonged PR interval. Prolonged PR interval for age on electrocardiography.
- Increased ESR. Elevated peak erythrocyte sedimentation rate during acute illness ≥60 mm/h and/or C-reactive protein ≥3.0 mg/dl.
Assessment and Diagnostic Findings
Although there’s no single test for rheumatic fever, diagnosis is based on medical history, physical exam and certain test results
- Throat culture. Throat cultures for GABHS infections usually are negative by the time symptoms of rheumatic fever or rheumatic heart disease (RHD) appear; make attempts to isolate the organism prior to the initiation of antibiotic therapy to help confirm a diagnosis of streptococcal pharyngitis and to allow typing of the organism if it is isolated successfully.
- Rapid antigen detection test. This test allows rapid detection of group A streptococci (GAS) antigen, allowing the diagnosis of streptococcal pharyngitis to be made and antibiotic therapy to be initiated while the patient is still in the physician’s office.
- Antistreptococcal antibodies. Clinical features of rheumatic fever begin when antistreptococcal antibody levels are at their peak; thus, these tests are useful for confirming previous GAS infection; antistreptococcal antibodies are particularly useful in patients who present with chorea as the only diagnostic criterion.
- Acute-phase reactants. C-reactive protein and erythrocyte sedimentation rate are elevated in individuals with rheumatic fever due to the inflammatory nature of the disease; both tests have high sensitivity but low specificity for rheumatic fever.
- Heart reactive antibodies. Tropomyosin is elevated in persons with acute rheumatic fever.
- Rapid detection test for D8/17. This immunofluorescence technique for identifying the B-cell marker D8/17 is positive in 90% of patients with rheumatic fever and may be useful for identifying patients who are at risk of developing rheumatic fever.
- Chest radiography. Cardiomegaly, pulmonary congestion, and other findings consistent with heart failure may be observed on chest radiograph in individuals with rheumatic fever.
- Echocardiography. In individuals with acute RHD, echocardiography identified and quantitated valve insufficiency and ventricular dysfunction.
Medical Management
Therapy is directed towards eliminating the GABHS pharyngitis (if still present), suppressing inflammation from the autoimmune response, and providing supportive treatment of congestive heart failure (CHF).
- Anti-inflammatory. Treatment of the acute inflammatory manifestations of acute rheumatic fever consists of salicylates and steroids; aspirin in anti-inflammatory doses effectively reduces all manifestations of the disease except chorea, and the response typically is dramatic.
- Corticosteroids. If moderate to severe carditis is present as indicated by cardiomegaly, third-degree heart block, or CHF, add PO prednisone to salicylate therapy.
- Anticonvulsant medications. For severe involuntary movements caused by Sydenham chorea, your doctor might prescribe an anticonvulsant, such as valproic acid (Depakene) or carbamazepine (Carbatrol, Tegretol, others).
- Antibiotics. Your child’s doctor will prescribe penicillin or another antibiotic to eliminate remaining strep bacteria.
- Surgical care. When heart failure persists or worsens after aggressive medical therapy for acute RHD, surgery to decrease valve insufficiency may be lifesaving; approximately 40% of patients with acute rheumatic fever subsequently develop mitral stenosis as adults.
- Diet. Advise nutritious diet without restrictions except in patients with CHF, who should follow a fluid-restricted and sodium-restricted diet; potassium supplementation may be necessary because of the mineralocorticoid effect of corticosteroid and the diuretics if used.
- Activity. Initially, place patients on bed rest, followed by a period of indoor activity before they are permitted to return to school; do not allow full activity until the APRs have returned to normal; patients with chorea may require a wheelchair and should be on homebound instruction until the abnormal movements resolve.
Pharmacologic Management
Treatment and prevention of group A streptococci pharyngitis outlined here are based on the current recommendations of the American Heart Association Practice Guidelines on Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute Streptococcal Pharyngitis.
- Antibiotics. The roles for antibiotics are to (1) initially treat GABHS pharyngitis, (2) prevent recurrent streptococcal pharyngitis, rheumatic fever (RF), and rheumatic heart disease (RHD), and (3) provide prophylaxis against bacterial endocarditis.
- Anti-inflammatory agents. Manifestations of acute rheumatic fever (including carditis) typically respond rapidly to therapy with anti-inflammatory agents; aspirin, in anti-inflammatory doses, is DOC; prednisone is added when evidence of worsening carditis and heart failure is noted.
- Therapy for congestive heart failure. Heart failure in RHD probably is related in part to the severe insufficiency of the mitral and aortic valves and in part to pancarditis; therapy traditionally has consisted of an inotropic agent (digitalis) in combination with diuretics (furosemide, spironolactone) and afterload reduction (captopril).
Nursing Management
Nursing care of a child with rheumatic fever include:
Nursing Assessment
Nursing assessment for a child with rheumatic fever are as follows:
- History. Obtain a complete up-to-date history from the child and the caregiver; ask about a recent sore throat or upper respiratory infection; find out when the symptoms began, the extent of the illness, and what if any treatment was obtained.
- Physical exam. Begin with a careful review of all systems, and note the child’s physical condition; observe for any signs that may be classified as major or minor manifestations; in the physical exam, observe for elevated temperature and pulse, and carefully examine for erythema marginatum, subcutaneous nodules, swollen or painful joints, or signs of chorea.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Acute pain related to joint pain when extremities are touched or moved.
- Deficient diversional activity related to prescribed bed rest.
- Activity intolerance related to carditis or arthralgia.
- Risk for injury related to chorea.
- Risk for noncompliance with prophylactic drug therapy related to financial or emotional burden of lifelong therapy.
- Deficient knowledge of caregiver related to the condition, need for long-term therapy, and risk factors.
Nursing Care Planning and Goals
Main Article 4 Acute Rheumatic Fever Nursing Care Plans
The major nursing care planning goals for rheumatic fever are:
- Reducing pain.
- Providing diversional activities and sensory stimulation.
- Conserving energy.
- Preventing injury.
Nursing Interventions
Nursing interventions for a child with rheumatic fever include:
- Provide comfort and reduce pain. Position the child to reduce joint pain; warm baths and gentle range-of-motion exercises help to alleviate some of the joint discomforts; use pain indicator scales with children so they are able to express the level of their pain.
- Provide diversional activities and sensory stimulation. For those who do not feel very ill, bed rest can cause distress or resentment; be creative in finding diversional activities that allow bed rest but prevent restlessness and boredom, such as a good book; quiet games can provide some entertainment, and plan all activities with the child’s developmental stage in mind.
- Promote energy conservation. Provide rest periods between activities to help pace the child’s energies and provide for maximum comfort; if the child has chorea, inform visitors that the child cannot control these movements, which are as upsetting to the child as they are to others.
- Prevent injury. Protect the child from injury by keeping the side rails up and padding them; do not leave a child with chorea unattended in a wheelchair, and use all appropriate safety measures.
Evaluation
Goals are met as evidenced by:Reducing pain.
- Providing diversional activities and sensory stimulation.
- Conserving energy.
- Preventing injury.
Documentation Guidelines
Documentation in a child with rheumatic fever includes:
- Baseline and subsequent assessment findings to include signs and symptoms.
- Individual cultural or religious restrictions and personal preferences.
- Plan of care and persons involved.
- Teaching plan.
- Client’s responses to teachings, interventions, and actions performed.
- Attainment or progress toward the desired outcome.
- Long-term needs, and who is responsible for actions to be taken.
Practice Quiz: Rheumatic Fever
Here’s a 5-item quiz for Rheumatic Fever study guide. Please visit our nursing test bank page for more NCLEX practice questions.
1. Which of the following instructions would Nurse Courtney include in a teaching plan that focuses on initial prevention for Sheri who is diagnosed with rheumatic fever?
A. Providing an antibiotic before dental work.
B. Treating streptococcal throat infections with an antibiotic
C. Giving penicillin to patients with rheumatic fever.
D. Using corticosteroid to reduce inflammation.
1. Answer: B. Treating streptococcal throat infections with an antibiotic.
- Option B: Rheumatoid fever results from improperly treated group beta-hemolytic streptococcal infections, usually pharyngitis. Therefore, prompt treatment of streptococcal throat infections with an antibiotic is a key preventive measure.
- Option A: An antibiotic is given to children with cardiac disease to prevent carditis, not rheumatic fever.
- Option C: Initial prevention is not possible once the child has rheumatic fever. However, the child will be treated with penicillin to prevent a recurrence of streptococcal infections.
- Option D: A corticosteroid may be used to reduce inflammation during treatment of rheumatic fever, not as a preventive measure.
2. A child is admitted to the hospital with a suspected rheumatic fever. Which of the following observations is NOT confirming of the diagnosis?
A. A history of a sore throat that was self-limited in the past month.
B. A reddened rash visible over the trunk and extremities.
C. An unexplained fever.
D. A negative antistreptolysin O titer.
2. Answer: D. A negative antistreptolysin O titer.
- Option D: Rheumatic fever is caused by an untreated group A B hemolytic Streptococcus infection in the previous 2-6 weeks, confirmed by a positive antistreptolysin O titer.
- Options A, B, C: Rheumatic fever is characterized by a red rash over the trunk and extremities as well as fever and other symptoms.
3. Molly, with suspected rheumatic fever, is admitted to the pediatric unit. When obtaining the child’s history, the nurse considers which information to be most important?
A. A fever that started 3 days ago.
B. A recent episode of pharyngitis.
C. Lack of interest in food.
D. Vomiting for 2 days.
3. Answer: B. A recent episode of pharyngitis.
- Option B: A recent episode of pharyngitis is the most important factor in establishing the diagnosis of rheumatic fever.
- Options A, C, D: Although the child may have a history of fever or vomiting or lack interest in food, these findings are not specific to rheumatic fever.
4. Which of the following organisms is responsible for the development of rheumatic fever?
A. Group A β-hemolytic streptococcus.
B. Staphylococcus aureus.
C. Streptococcal pneumonia.
D. Haemophilus influenza.
4. Answer: A. Group A β-hemolytic streptococcus.
- Option A: Rheumatic fever results from a delayed reaction to inadequately treated group A β-hemolytic streptococcal infection.
- Options B, C, D: These organisms are not responsible for rheumatic fever.
5. A 9-year-old is admitted with suspected rheumatic fever. Which finding is suggestive of polymigratory arthritis?
A. Painless swelling over the extensor surfaces of the joints.
B. Irregular movements of the extremities and facial grimacing.
C. Swelling, inflammation, and effusion of the joints.
D. Faint areas of red demarcation over the back and abdomen.
5. Answer: C. Swelling, inflammation, and effusion of the joints.
- Option C: The child with polymigratory arthritis will exhibit swollen, painful joints.
- Option A is incorrect because it describes subcutaneous nodules.
- Option B is incorrect because it describes Syndeham’s chorea.
- Option D is incorrect because it describes erythema marginatum.
See Also
Related topics to this study guide:
- Pediatric Nursing Study Guides
- Nursing Notes: Study Guides for Various Topics
- Pediatric Nursing NCLEX Practice Questions
Further Reading
Recommended resources and books for pediatric nursing:

